Alliance Pivots to Telemedicine
Alliance Medical Center is expanding its telemedicine services to help prevent the spread of COVID-19.
As we all work to prevent the spread of COVID-19 by staying home and limiting in-person interaction, our community health clinics like Alliance Medical Center are having to rethink the way they take care of their patients.
The first week of the Shelter in Place order, Alliance Medical Center’s behavioral health team switched all of their appointments to phone calls and then online video visits. Over the last two months, with support from the Healthcare Foundation’s Emergency Heathcare Fund, Alliance has expanded its telemedicine to include phone and video clinic visits, a texting platform to reach patients and remote monitoring devices like thermometer, diabetic monitoring equipment and digital blood pressure cuffs.
While there are new challenges to this approach to treatment, Susannah Labbe, Alliance’s medical director and a pediatric nurse practitioner, says they have discovered some amazing advantages. One family that she regularly treats had a child with a rash. The mother was able to show the rash to Susannah by video and then all of the children crowded into the video to say hi.
“All five of the kids were waving to me and excited to see me,” she says. “It’s a really positive thing when we can bring the care into their home.”
Normally this mother would have had to bring all of her children into the clinic to have the rash looked at, Susannah explains. That’s something they don’t want patients to do right now with COVID-19 in the community, but it’s also not ideal during regular cold and flu season.
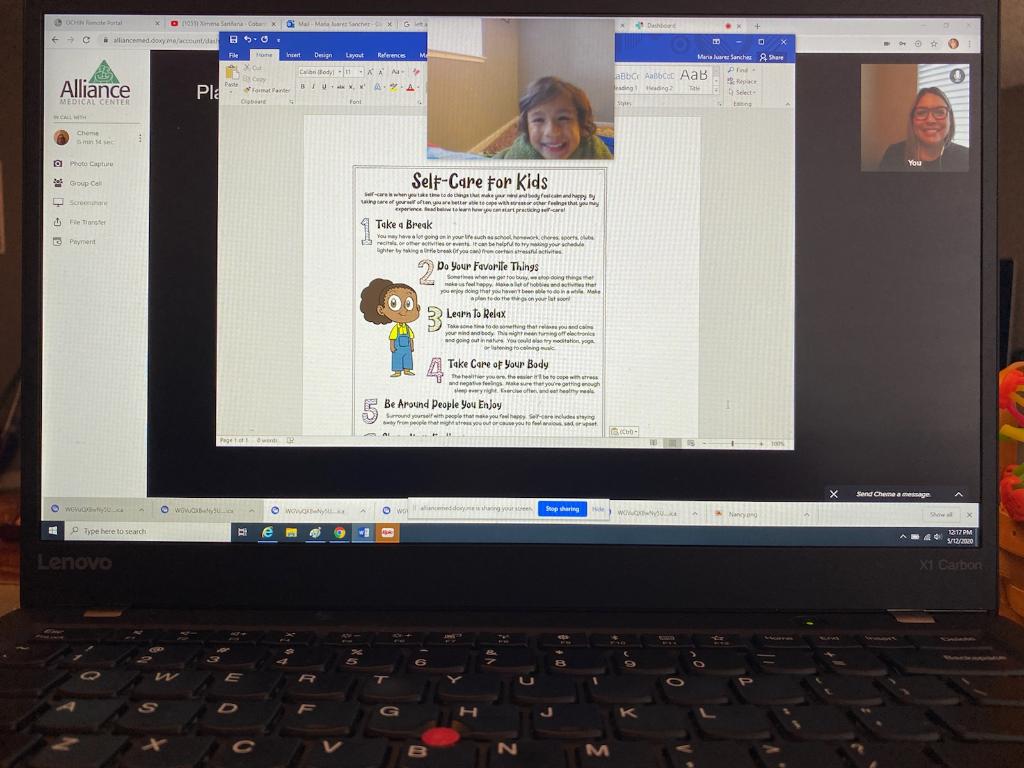
Another mother called crying hysterically after her toddler fell and cut its lip while practicing walking. Susannah got the baby and the mother onto a video call and was able to examine the baby’s injury and calm the mother down. Susannah could see that the baby did not need stitches and by the end of the call the baby was so fascinated by the nurse practitioner on the screen that it didn’t want to give up the phone.
Alliance serves 13,000 patients throughout northern Sonoma County. The majority of its patients are economically disadvantaged and 55 percent are monolingual Spanish speakers. “The needs haven’t necessarily changed” with COVID-19, Susannah says, “it’s just made the health disparities of this population even more glaringly evident.”

Her patients don’t have sick time or are afraid to stay home and lose work, she says. They’re worried about homelessness and feeding their families, she adds. And they “have the full gamut of medical concerns but with very limited resources to address them.”
Many patients have poorly controlled hypertension, according to Susannah, which can lead to heart attacks, strokes and kidney failure. A cardiologist at Alliance had already been using a self-monitoring blood pressure device with her elderly mother who doesn’t live close by and felt confident that their patients could learn to check their own blood pressure.
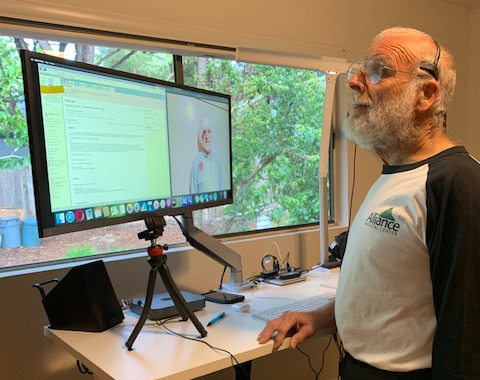
Now Alliance is distributing the devices along with instructions on how to use it, a log to track readings and a letter explaining why managing blood pressure is so important. A staff member schedules a follow-up appointment and a dietitian can also provide video visits. So far all of the patients with the new device have been using it successfully.
As Alliance staff and patients get used to these new conditions, there are other looming concerns. Susannah says she’s expecting a significant increase in Medi-Cal enrollment as people lose jobs and insurance. She’s also worried about some of the preventative care services they aren’t able to provide right now like cancer screenings, well child visits and regular immunizations (children under two have been receiving their vaccines). As the state of California begins to lift restrictions, one of the next challenges will be getting people back into the clinics and making sure they feel safe enough to get the preventative care they need, she says.

Related News + Stories
Invest in Our Community
Your support is vital to our collective vision of eliminating health inequities in northern Sonoma County.
Donate